Current research on dissociation builds on a tradition dating back to Janet’s (1887) distinction between psychological phenomena, or psychoform dissociative symptoms, and bodily phenomena, or somatoform dissociative symptoms. FND is typically understood to primarily involve the latter (Nijenhuis et al., 1996; Pick et al., 2017; Vuilleumier & Cojan, 2011).
Explanations for why individuals with FND are experientially disconnected from their bodies are manifold: dissociation as a survival response to trauma; cultural, familial, or religious reasons; alexithymia (difficulty identifying feelings and distinguishing between feelings and the bodily sensations of emotional arousal); or impaired interoception (the ability to sense the internal states of the body). The most widely accepted contributing etiologic factor, however, is prior exposure to chronic stress and trauma.
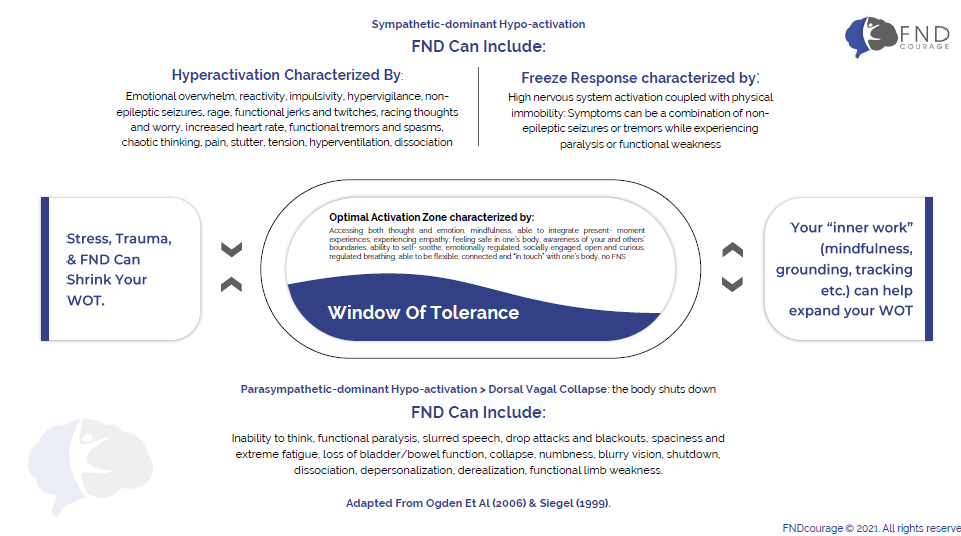
Dr. Moenter talks about dissociation happening on a continuum from “spacing out” to out-of-body experiences and full dissociative states such as non-epileptic seizures. The healing process involves learning how to self-regulate dissociative states early so as to not fully disconnect from the present moment experience. The ability to stay present allows for a greater capacity to be mindful of changes in nervous system activation (FND symptoms).
Non-epileptic seizures (NES), also called dissociative seizures or functional seizures are often part of FND. Functional seizures can be viewed as an expression of a sympathetically over-activated nervous system. Dr. Moenter views functional seizures as a “reset mechanism” preventing the prolonged overactivation of the nervous system which could potentially lead to more severe psycho-physiological damages.
A typical feature of functional seizures is involuntary movement that resembles epileptic seizures. Those movements can be micro-movements (twitches, spasms, subtle shaking etc.) or macro-movements (visible large movements of the limps, head, upper or lower body) often with loss of consciousness. Some individuals have described still having self-awareness but not being able to react to the environment (responding to people asking questions, or protecting oneself from physical harm) while also not being able to self-regulate their nervous system enough to stop the seizure activity.
For some individuals with FND, symptoms are more pronounced in the realm of a hypo-activated nervous system (not enough activation). When the nervous system is in a state of parasympathetic-dominant Hypo-activation (or dorsal vagal collapse), the body shuts down. This shut-down can be experienced as partial or full paralysis or weakness.
Other symptoms that can accompany the dorsal vagal collapse can be the inability to think, slurred speech, drop attacks and blackouts, spaciness and extreme fatigue, loss of bladder/bowel function, collapse, numbness, depersonalization, or derealization.
Many individuals with FND experience sensory sensitivities or sensory symptoms. Sensory sensitivities can impact all senses (touch, smell, sound, taste, vision, and interoception). Lights can feel too bright, touch uncomfortable or even painful, sounds intrusive, smells overpowering, taste intolerable and the ability to sense inner body sensations (interoception) is often lacking.
The central nervous system is designed to filter out redundant and unnecessary stimuli and organize sensorimotor information into an integrated experience. This process is called the “gating mechanism,” and it may be dysregulated in many clients with FND who describe a variety of sensory challenges that manifest as over-sensitivity or under-sensitivity.
Over-sensitivity, or “sensory overload,” implies a heightened sensitivity to touch, sounds, sights, textures, smells, and other sensory stimuli. Under-sensitivity can manifest as a lack of responsiveness to factors such as temperature, touch, or noise. It is possible that these symptoms are caused by sensorimotor gating impairments that prevent individuals from integrating information from internal and external sources as normal.
Dr. Moenter explains how sensory processing works and how you can regulate and increase your ability to be with sensory stimuli. Learning about the gating mechanism of the brain, your boundary style, and concrete boundary tools might increase your ability to process sensory stimuli and feel less negatively impacted by sensory stimuli.
Trauma is the result of experiencing inescapably stressful events that overwhelm an individual’s existing coping mechanisms while obstructing information-processing abilities. It affects memory in two ways, modifying both sensorimotor and affective levels of memory formation and recall and often producing the symptoms of somatoform and psychoform as seen in FND.
Some individuals with FND have experienced chronic stress or trauma prior to the onset of FND. The exposure to life-altering adverse events can contribute to the dysregulation of the autonomic nervous system. Since FNDcourage is based on the idea that FND is an expression of a dysregulated nervous system (too much or too little activation), part of the healing process is undoubtedly the work with and resolution of any adverse nervous system changes resulting from chronic stress and/or trauma.
Although a direct causal connection between trauma and the onset of FND has not yet been identified, trauma is widely believed to be a contributing factor, alongside adverse childhood experiences (ACE). For instance, several studies have concluded that individuals with FND exhibit elevated rates of post-traumatic stress disorder (PTSD), and those with FND display disproportionately high incidence of involuntary dissociative states.
You will learn about resilience and how to increase your on resilience in the face of stressful external and internal experiences. Resilience is your ability to quickly and fully recover from challenging, stressful, and traumatic events.
Being resilient means you have the capacity to face stressors, to lean into discomfort, instead of avoiding challenges. Part of the model of how Dr. MOenter works is to NOT use the word “triggers.” Many professionals talk about “triggers” in the context of FND. What Dr. Moenter has seen in her work with FND is that people naturally orient away from “triggers” creating a pattern of avoidance. Such avoidance, over time, leads to a very limited lifestyle and a lack of trust and strength necessary to lean into the discomfort of FND, which eventually will help reduce symptoms.
Dr. Moenter introduces the concept of “precursors” feelings, thoughts, and physical sensations that can be an indicator that your nervous system is at the beginning stages of dysregulation.
“True freedom means living our lives fully, not avoiding, not “coping,” but truly developing the capacity to be with all that life offers us.” Afra Moenter, Ph.D.
Functional Movement Disorders can be divided into tremors, twitches and jerks, gait problems (difficulty walking), functional weakness. These functional symptoms are not caused by damage or disease of the nervous system.
Dr. Moenter talks about involuntary and voluntary movements, and how to relate to and potentially ease involuntary symptoms in your body.
Dr. Moenter explores emotional imbalances as part of FND. Research shows that individuals with FND have
Common emotions that individuals with FND feel are shame, anxiety, despair, hopelessness, helplessness, and fear. Dr. Moenter’s explains how emotions can be an expression of a regulated (sadness, curiosity, anger, fear etc.) or a dysregulated (terror, rage, shame, obsession etc.) nervous system. As part of the FNDcourage course you will learn how to identify your emotions as they relate to your nervous system activation and learn how to self-regulate your emotional state. Such emotional self-regulation can positively impact your functional neurological symptoms.
Dr. Moenter also explores how emotions contribute to your body posture, how you hold yourself in your body, and how in turn that experience might make you more susceptible to certain FND symptoms. By learning about and changing your Emotional Anatomy (Stanley Keleman) you will increase your interoception (body awareness) and increase your ability to regulate your nervous system.
Many individuals with FND describe functional cognitive symptoms. Symptoms vary, but can often include:
If you experience any of these symptoms as part your FND, your challenges might not be due to you loosing your intellectual capacity or curiosity. Dr. Moenter views cognitive symptoms as an often temporary limitation; potentially caused by severe dissociative states and/or a result of the chronic stress of FND (or other life-altering events). The exposure to chronic stress and trauma can impair the functionality of the pre-frontal cortex (responsible for executive function, decision making, etc.) and therefore can leave you with a limited capacity to think clearly or make sound decisions for yourself.
FNDcourage © 2025. All Rights Reserved.
| Cookie | Duration | Description |
|---|---|---|
| cookielawinfo-checbox-analytics | 11 months | This cookie is set by GDPR Cookie Consent plugin. The cookie is used to store the user consent for the cookies in the category "Analytics". |
| cookielawinfo-checbox-functional | 11 months | The cookie is set by GDPR cookie consent to record the user consent for the cookies in the category "Functional". |
| cookielawinfo-checbox-others | 11 months | This cookie is set by GDPR Cookie Consent plugin. The cookie is used to store the user consent for the cookies in the category "Other. |
| cookielawinfo-checkbox-necessary | 11 months | This cookie is set by GDPR Cookie Consent plugin. The cookies is used to store the user consent for the cookies in the category "Necessary". |
| cookielawinfo-checkbox-performance | 11 months | This cookie is set by GDPR Cookie Consent plugin. The cookie is used to store the user consent for the cookies in the category "Performance". |
| viewed_cookie_policy | 11 months | The cookie is set by the GDPR Cookie Consent plugin and is used to store whether or not user has consented to the use of cookies. It does not store any personal data. |